Folate deficiency may come as a surprise, considering just how widely available folate – and its synthetic version, folic acid – is. It’s found in many foods, from fruits and veggies to eggs, meat, and seafood! It’s also added to grain products (rice, cereal, pasta, bread) in many countries as part of folic acid fortification programs.
So, why is folate deficiency still a thing? Who’s at risk of becoming deficient, and what are the symptoms to watch out for? And more importantly, what’s the best way to prevent and treat this condition (hint: our 5-MTHF supplement can help)? We’ll answer all these questions – and more – in this blog post.
Table of Contents
What’s folate anyway and why is it so important?
Before we go into the specifics of folate deficiency, let’s first understand what it is and why it’s essential to maintain healthy levels.
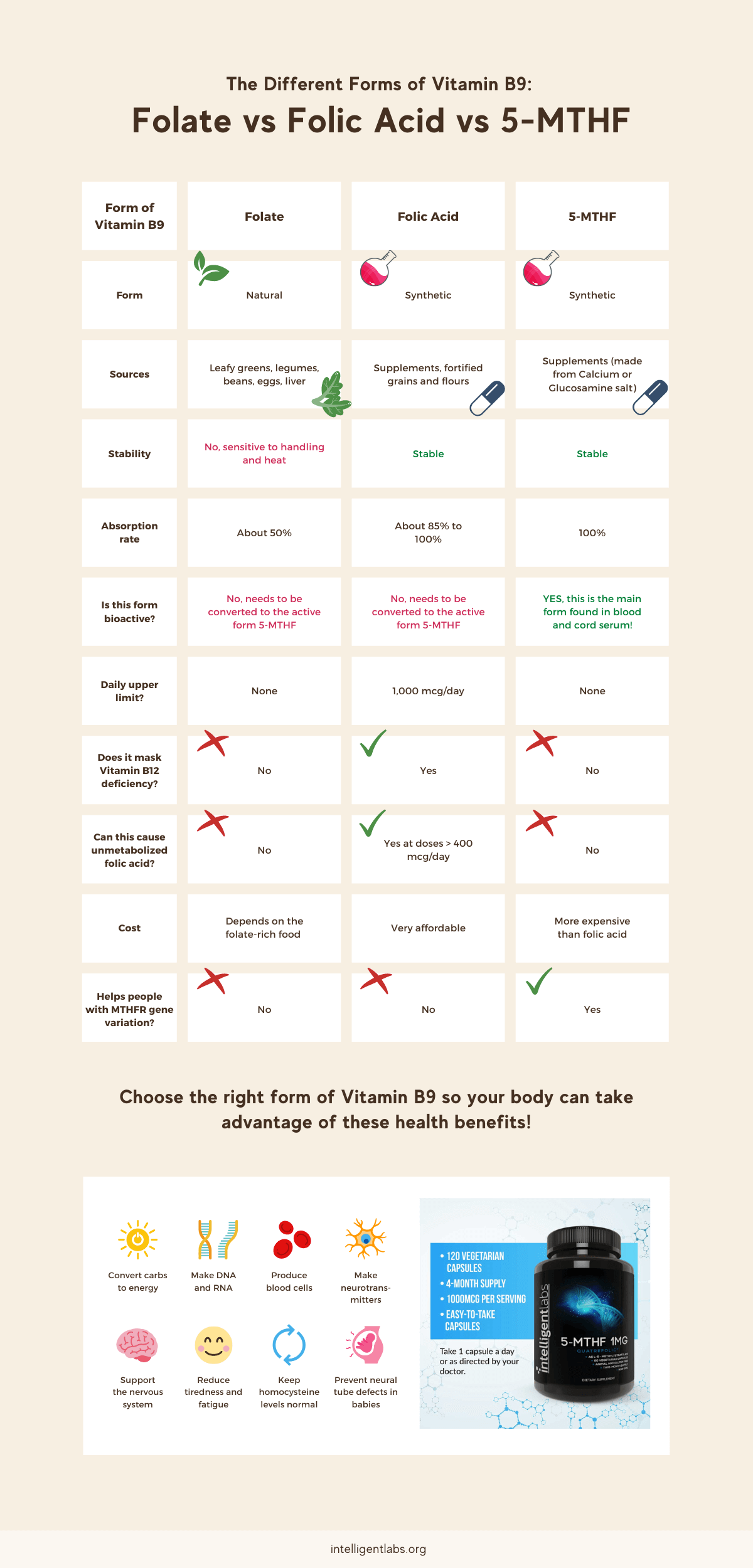
Folate, folic acid, and 5-MTHF activated folic acid are all just different forms of vitamin B9.
Folate is the natural form found in foods. Folic acid is the synthetic or man-made version. And 5-MTHF activated folic acid is the form found in blood serum, meaning BOTH folate and folic acid are converted to 5-MTHF in the body.
Unfortunately, many people cannot efficiently convert folate and folic acid into 5-MTHF due to a variation in the MTHFR gene.
The solution? Take 5-MTHF in supplement form. Since 5-MTHF is already the bioactive form, it’s readily absorbed by the body. No conversions are needed. Doing so allows these individuals to take advantage of folate’s health benefits readily!
Here’s an infographic summarizing the different forms of vitamin B9:
How to recognize the signs and symptoms of folate deficiency?
Diagnosing a folate deficiency is best left to professionals, aka your doctor. They may need to carry out a blood test to measure your folate levels accurately. Moreover, many folate deficiency symptoms overlap with other vitamin B deficiencies (there are eight vitamins in the B complex).
That said, here are some of the most common symptoms of folate deficiencies to look out for (1):
- Anemia – this has its own set of symptoms, most notably, paleness, dizziness, and shortness of breath
- Extreme fatigue
- Mouth sores or ulcers
- Red and swollen tongue
- Brain fog
- Memory loss
- Depression
- Heart palpitations
- Muscle weakness
- Premature hair graying
Mothers who give birth to babies with birth defects may also be deficient in folate. We highly recommend taking 5-MTHF activated folic acid for prenatal health to support a healthy pregnancy!
What causes folate deficiency and who’s at risk?
The main cause of folate deficiency is simple enough, and that is not getting enough folate for the body’s needs.
As for who’s at risk, the first on the list are those who don’t get enough folate or folic acid from their diet.
Next are individuals with the MTHFR gene variation since they cannot efficiently convert the folate they eat into the active form (5-MTHF).
Also, pregnant and lactating women need higher-than-normal folate levels, too. So, women planning to conceive must build up their folate levels months before conception; this prevents neural tube defects in a developing fetus.
People in their 50s may also want to load up on their folate intake as aging and certain medications may cause malabsorption. Folate deficiency in older individuals increases the risk of Alzheimer’s and dementia (2).
People with Crohn’s, Celiac, or inflammatory bowel disease may also be prone to low folate levels since they may not absorb folate well (3)(4). Similarly, excessive alcohol drinkers and those who follow very restrictive diets are also at risk (5).
How to treat folate deficiency and raise blood folate levels?
There are a few ways to get your folate levels up:
First is to eat a healthy, balanced diet that includes folate-rich foods. Be mindful of your cooking method though, as heat easily destroys folate (6).
Second, eating folic acid-enriched food is also a good idea.
The third way is to take folic acid supplements. However, you need to be cautious when taking folic acid. Too much can lead to unmetabolized folic acid, which may mask a vitamin B12 deficiency and pernicious anemia (7).
Of course, the three options above will likely only benefit those who do not have the MTHFR gene variation. If you’ve got this issue, the best way to get your folate levels up is to take a 5-MTHF supplement.
Unlike regular folic acid supplements, 5-MTHF supplements are absorbed fully, so they do not lead to unmetabolized folic acid. 5-MTHF supplements also will not mask a vitamin B12 deficiency (8).
How much folate or folic acid to take daily and prevent deficiency?
Here’s the recommended daily amount for taking folic acid (9):
| Life Stage | Recommended amount |
| Birth to 6 months | 65 mcg DFE |
| Infants 7-12 months | 80 mcg DFE |
| Children 1-3 years | 150 mcg DFE |
| Children 4-8 years | 200 mcg DFE |
| Children 9-13 years | 300 mcg DFE |
| Teens 14-18 years | 400 mcg DFE |
| Adults 19+ years | 400 mcg DFE |
| Pregnant teens and women | 600 mcg DFE |
| Breastfeeding teens and women | 500 mcg DFE |
Note: 1 mcg DFE is equal to:
- 1 mcg food folate
- 0.6 mcg folic acid from fortified foods or supplements (when consumed with food)
- 0.5 mcg folic acid from supplements (when taken on an empty stomach)
How long does it take to correct or treat a folate deficiency?
Eating more folate-rich foods and supplementing with folic acid or 5-MTHF won’t reverse a deficiency overnight. However, the good news is that it will gradually improve, and folate levels should return to normal within 3-6 months (10).
Conclusion
Getting diagnosed with low folate levels or folate deficiency is not the end of the world. As you’ve learned in this article, taking 5-MTHF activated folic acid regularly may help increase your folate levels.
Before you start supplementing, however, it’s important to speak with your doctor. They should be able to advise you on the correct dosage and frequency of taking the supplement.




